Blood Transfusion and Regenerative Medicine
Mission
Regenerative medicine uses cells and artificial materials to regenerate damaged tissues and organs that have lost their function, and also to treat patients with malignant disorders or immunological abnormalities. It has the potential to bring about new medical treatments for injuries and illnesses that previously had no treatment. Regenerative medicine technology is also being used to clarify the causes of incurable diseases and develop medicines.
Blood Transfusion and Regenerative Medicine at Our Hospital
We are currently providing Autologous Peripheral Blood CD34-Positive Cell Transplantation for
- Patients with Chronic Severe Limb Ischemia (elective treatment)
- Patients with Chronic Kidney Disease (clinical research)
By providing regenerative therapy as an elective treatment (self-funded) or in clinical research, we committed to accumulate evidence of the efficacy and safety of regenerative medicine so that in the future, regenerative medicine will become a standard treatment and accessible to everyone.
Achievements
- In a clinical trial conducted in 2015 involving six dialysis patients with severe limb ischemia, a 100% amputation-free survival rate was achieved one year after autologous CD34-positive cell transplantation therapy (Ohtake T et al. Stem Cells Transl Med. 2018).
- In a clinical trial conducted from 2022 to 2023 involving patients with chronic progressive kidney disease, improvements in eGFR and intrarenal resistive index were observed in the initial study of four cases following autologous CD34-positive cell transplantation therapy (Ohtake T et al. World J Stem Cells. 2024).
Leading Expert
Dr. Ryuji Tanosaki brings world-class expertise in hematopoietic stem cell transplantation and transfusion/cell therapy. He is passionate about delivering safe, cutting-edge, and transformative therapies, including cell-based and regenerative medicine products. At our hospital, Dr. Tanosaki is working to establish robust support systems for patients with hematologic malignancies, such as lymphoma, leukemia, and multiple myeloma. He aims to develop advanced frameworks for next-generation immunotherapies, including CAR-T cell therapy, to ensure that patients have access to innovative and safe treatments.
BACKGROUND:
- Keio University School of Medicine, M.D. (1985)
- Assistant, Department of Hematology and Hematopoietic Stem Cell Transplantation, Keio University School of Medicine (1989–1995)
- Visiting Researcher, New York Blood Center, USA (1995)
- Staff Physician & Director, Hematopoietic Cell Transplantation, National Cancer Center Hospital (1997–2010)
- Deputy Director, Pathology & Clinical Laboratory, National Cancer Center Hospital (2010–2012)
- Director, Department of Transfusion Medicine, National Cancer Center Hospital (2012–2016)
- Professor, Center for Transfusion & Cell Therapy, Keio University (2016–2025)
- Director, Center of Blood Transfusion and Regenerative Medicine, Shonan Kamakura General Hospital (2025–present)
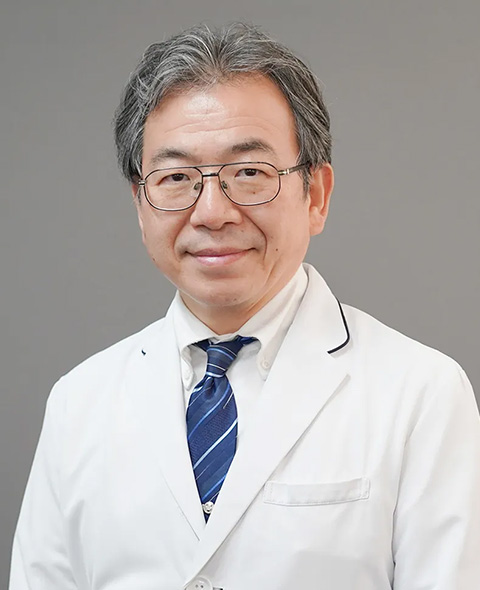
Ryuji Tanosaki
Director, Center of Blood Transfusion and Regenerative Medicine
Dr. Takayasu Ohtake specializes in vascular regenerative and anti-inflammatory treatments using EPCs. In 2015, he conducted a clinical trial with dialysis patients suffering from critical limb ischemia, achieving an 83% improvement rate from severe to mild disease and a 100% amputation-free survival rate (Ohtake T et al. Stem Cells Transl Med. 2018). He now offers elective treatment for patients with peripheral arterial disease not undergoing dialysis and has initiated trials for autologous CD34-positive cell therapy in acute renal failure and chronic kidney disease, showing promising results (Ohtake T et al. World J Stem Cells. 2024). Ongoing studies continue in Japan and internationally.
BACKGROUND:
- Hamamatsu University School of Medicine (1987)
- Hamamatsu University Hospital and Fujinomiya Municipal Hospital
- Head of Nephrology, Shonan Kamakura General Hospital (2002-2012)
- Chief Director of Nephrology, Immunology, and Vascular Medicine, Shonan Kamakura General Hospital (2012-2018)
- Deputy Hospital Director of Shonan Kamakura General Hospital (2018-present)
- Chief of Regenerative Medicine Department, Shonan Kamakura General Hospital (2018-present)

Takayasu Ohtake
Chief of Regenerative Medicine Department
&
Deputy Hospital Director of Shonan Kamakura General Hospital







